More Than a Bedroom Issue
Erectile dysfunction (ED) is often treated as a purely sexual or emotional issue, but in many cases, it’s actually an early warning sign of underlying health conditions. Because the erection process depends on blood flow, nerve function, hormone balance, and psychological well-being, any disruption in these systems can affect performance. That’s why ED is frequently the first noticeable symptom of deeper medical problems. Understanding this connection could save more than your sex life — it could save your life.
ED and the Cardiovascular System
One of the most important links between ED and general health is the connection to cardiovascular disease. Erections require healthy arteries and strong blood flow. When blood vessels are narrowed or damaged, it becomes harder to achieve and maintain an erection. This same issue — atherosclerosis — is what causes heart attacks and strokes. In fact, ED often appears 3 to 5 years before symptoms of heart disease. If you have ED, it may be a sign of:
- High blood pressure (hypertension)
- High cholesterol
- Coronary artery disease
- Peripheral artery disease
- Early-stage atherosclerosis
Doctors now consider ED a form of vascular dysfunction and a strong predictor of future cardiac events.
ED and Diabetes
Diabetes — especially when poorly managed — is another major cause of erectile dysfunction. High blood sugar damages blood vessels and nerves, which impairs blood flow and sensation. Up to 75% of men with diabetes experience some degree of ED. If you’ve been struggling with erections and also notice excessive thirst, fatigue, blurry vision, or frequent urination, it’s worth checking your blood glucose levels. Prediabetes and insulin resistance can also contribute to ED, even before full diabetes develops.
ED and Hormonal Imbalances
Low testosterone is a well-known contributor to ED. This condition, called hypogonadism, can result from aging, obesity, metabolic issues, or other health conditions. Symptoms may include low libido, fatigue, irritability, loss of muscle mass, and poor concentration. Thyroid problems and high prolactin levels can also interfere with sexual performance. If you suspect hormones are affecting your erections, ask your doctor about a full hormonal panel to evaluate testosterone, free testosterone, estradiol, and thyroid function.
ED and Mental Health
Your mind plays a key role in sexual arousal. Conditions such as depression, anxiety, PTSD, and chronic stress can all suppress libido, affect arousal, and lead to erectile problems. ED can also cause or worsen these same conditions, creating a frustrating cycle. If your ED coincides with mood changes, low motivation, sleep problems, or irritability, don’t ignore it — treating mental health often leads to improvements in sexual function as well.
ED and Sleep Disorders
Sleep is essential for testosterone production, nitric oxide synthesis, and nerve regeneration. Men with sleep apnea often suffer from ED due to repeated drops in oxygen levels and chronic fatigue. Snoring, choking during sleep, or extreme daytime sleepiness are red flags. Treating sleep apnea with a CPAP machine or improving sleep hygiene can lead to significant improvements in erections and energy.
ED and Obesity
Excess body fat, especially around the abdomen, reduces testosterone levels, increases estrogen, and promotes inflammation — all of which contribute to ED. Obesity is also linked to insulin resistance, poor circulation, and reduced self-esteem. Losing weight, even modestly, often improves erectile function and overall vitality.
ED and Neurological Conditions
Diseases that affect the brain or nervous system can interfere with the signals that trigger erections. These include:
- Multiple sclerosis
- Parkinson’s disease
- Stroke
- Spinal cord injuries
- Alzheimer’s disease
If you’ve experienced neurological symptoms like tremors, numbness, weakness, or changes in coordination, mention them to your doctor along with any issues with erections.
ED and Medications
Certain medications have side effects that include erectile dysfunction. Common culprits include:
- Antidepressants (especially SSRIs)
- Blood pressure medications (like beta-blockers and diuretics)
- Antihistamines
- Opioid painkillers
- Hormone therapies for prostate cancer
If you noticed ED after starting a new medication, talk to your doctor about possible alternatives or dosage adjustments.
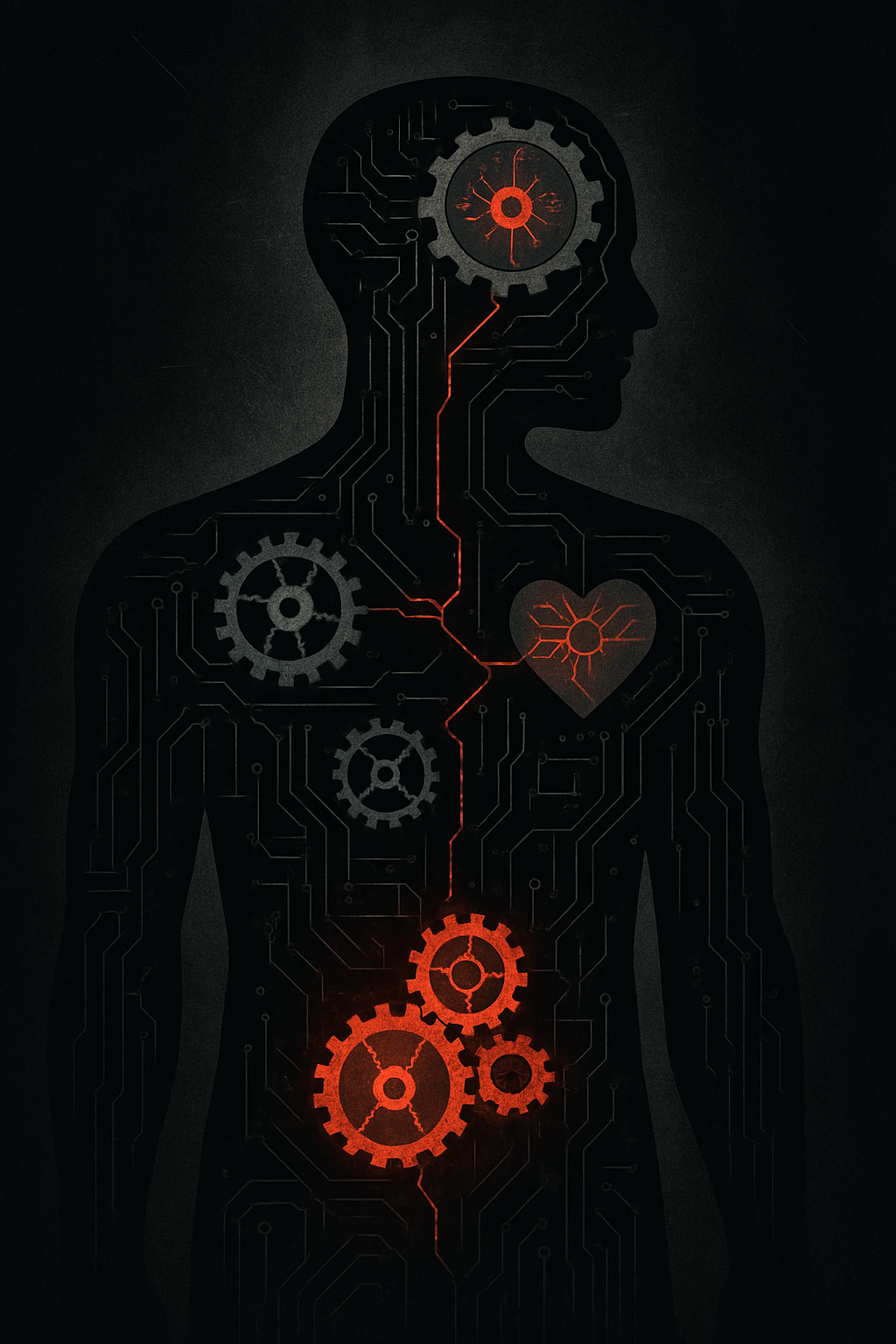
ED as a Health Check Engine Light
Think of ED as your body’s warning system. Just like a check engine light in your car, it signals that something needs attention. Instead of ignoring it or only treating the symptoms with pills, use it as an opportunity to improve your total health. The benefits will go far beyond the bedroom — they’ll extend to your heart, brain, mood, and longevity.
When to See a Doctor
If you’ve experienced ongoing ED for more than a few weeks, schedule an appointment with a healthcare provider. They may order tests to check:
- Blood pressure
- Cholesterol and triglyceride levels
- Blood sugar (A1C)
- Testosterone and other hormones
- Kidney and liver function
- Sleep quality and mental health status
A full evaluation can uncover hidden problems early and give you the tools to address them before they become serious.
Treat the Cause, Not Just the Symptom
While medications like sildenafil or tadalafil can provide short-term help, they don’t solve the underlying problem. Long-term solutions come from improving your overall health — through nutrition, exercise, sleep, stress management, and medical support. Erectile dysfunction isn’t just a sexual issue — it’s a whole-body signal that something deeper may need care.